RCM CYCLE STPES
RCM CYCLE
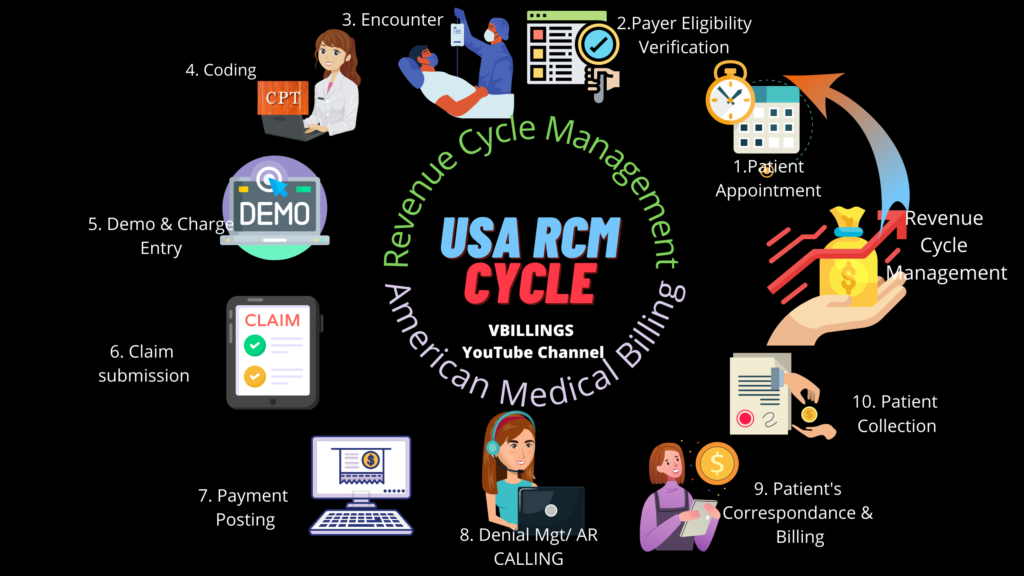

Steps in RCM Cycle
There are the most common 9 steps that involve in the RCM cycle
- Patent appointment/Preregistration
- Eligibility and Insurance Benefits verification
- Encounter
- Medical Coding
- Demo & Charge Entry
- Claim Submission
- Payment Posting
- Denial Management/AR Followup
- Patient Correspondance sending
- Patient Collections.
1. Patent appointment/Preregistration
In Revenue Cycle Management (RCM) patient’s appointment is the first step. A patient can get a doctor’s appointment by call, online, or by visiting the doctor’s office/hospital. The patient or member should call for an appointment at least 48 hours prior. Once the Appointment is scheduled, necessary information like patient details, insurance details, the reason for visit, etc are noted down by the front desk rep.
2. Eligibility and Insurance Benefits verification
After the patient’s appointment, patient eligibility and benefits are checked with patient insurance to verify that the services that the patient will get are covered or not by insurance. Other details like Copay, Coinsurance, Deductible, and Prior authorization in this process.
3. Encounter
Once eligibility and benefits verification was completed, the patient will get the treatment from the doctor at the scheduled time. The treatment given to the patient is recorded on the superbill, EMR, or in the form of voice (Dicta Phone), etc.
4. Medical Coding
The coding team read the medical records and creates coding. On the claim form patient Diagnosis (ICD), Current Procedural Terminology (CPT), and Healthcare Common Procedure Coding System (HCPCS) are used.
5. Demo & Charge Entry
Once all the essential information is gathered, it’s time to enter those data on the claim form or in the billing software. Here the claim form will be created with all the billing details, service details, provider details, patient details, and insurance details. A claim form can be filled in by hand or via using billing software.
6. Claim Submission
After the chargee entry, it’s time to send the claim form to the insurance company to get paid for the services rendered by the Healthcare providers 3 types of claim submissions: 1. Paper claim submission 2. Electronic claim submission 3. Online claim entry on an insurance web portal.
6. Payment Posting
When the claim gets approved for payment, the insurance company sends paid EOB or ERA along with the payment. Payment will be issued through different modes of transmission: 1. Paper Check 2. EFT (Electronic Fund Transfer) 3. Virtual Credit card. The EOB is posted manually or electronically by the payment posting team.
8. Denial Management/AR Followup
This process includes Insurance follow-ups, claims status checks, resolution of denied/rejected claims, preparing appeal letters, etc.
9. Patient Correspondance sending
After the EOB has been received from the payer, now biller will make the statement for the patient. After the payer has paid the provider for a portion of the services on the claim as per the contract, the remaining portion is passed to the patient. A biller may include an EOB with the statement. EOBs can be useful in explaining to the patient why certain services were covered while others were not.
10. Patient Collections
It is the process of collecting the payment from the patient when there is reduced reimbursement from the payers, it means the health plan does not cover all the services. This is the duty of the billers to send those outstanding payments to the patient by generating a Patient statement and follow-up. Follow-up may involve contacting the patient directly and sending follow-up bills. In worst-case scenarios, at last, collection agency follow-ups until the patients finally pay up.
