Medically Not Necessity Denial
Medical necessity is defined as accepted health care services and supplies provided by healthcare entities appropriate to evaluating and treating a disease, condition, illness, or injury and consistent with the applicable standard of care.
For example: If a patient visited a provider with a Stomach-Ache and was diagnosed with a Stomach infection, but the provider billed the payer for a Chest x-ray, now the payer would deny the claim as medically not necessary because patients who don’t have any chest-related problems or symptoms.
Claim Adjustment and Remark Codes:
C O 50: These are non-covered services because this is not deemed a “medical necessity” by the payer.
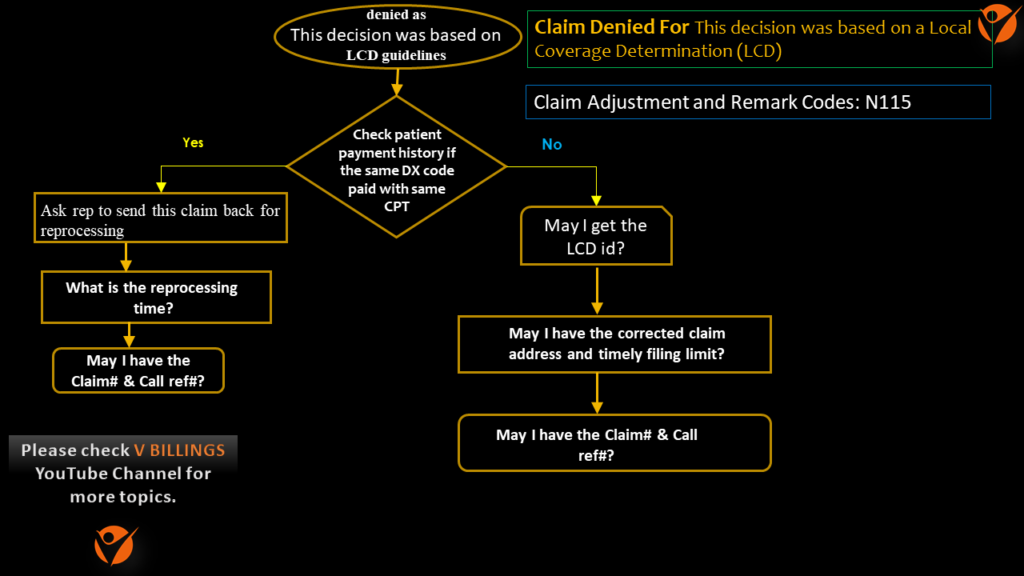
N 1 1 5: This decision was based on a Local Coverage Determination (LCD). An L C D provides a guide to assist in determining whether a particular item or service is covered.
Reasons:
1. The treatment does not appear to meet medical necessity criteria
2. The treatment cannot be medically certified based on the information provided by the treating clinician, or the treating clinician’s designated representative.
3. The procedure code is billed with an incompatible diagnosis
4. Payment purposes and the ICD-10 code(s) submitted are not covered under a Local or National Coverage Determination (LCD/NCD).
Steps to resolve :
1. LCDs specify under what clinical circumstances a service is considered to be reasonable and necessary for the diagnosis or treatment of illness or injury, or to improve the functioning of a malformed body part.
2. Refer to LCD and procedure to diagnosis lookup tool, to determine if a current and draft LCD exists for the denied procedure code.
3. If the LCD exists for the procedure code, need to call the insurance and request to reprocess.
4. If the LCD does not exist, need to check if there are any previously paid claims with the same set of codes for the same patient. If yes, need to call insurance and request to reprocess the claim.
5. If not, need to check with the insurance what are the documents acceptable as proof of Medical Necessity and send out an appeal with the relevant documents.
Note: This scenario can be worked upon without calling. Calling is needed only when we need the claim to be reprocessed by the insurance.
Flow Chart for Medically not necessity denial:
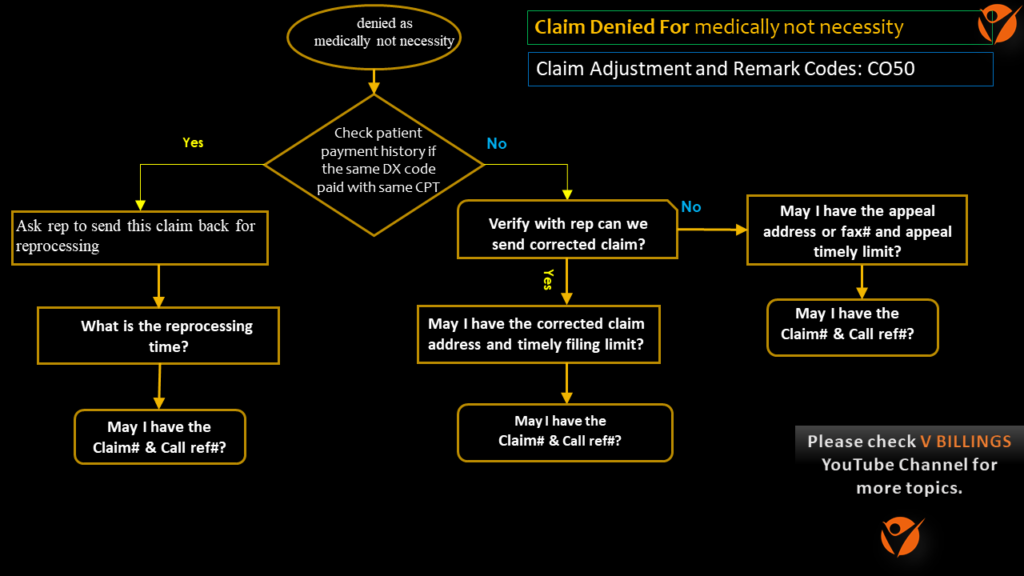
End action:
- Send to the coding team to review for correct dx code and once response received with correct DX details then send corrected claim to insurance by updating correct dx code.
- If the coding team mentioned that the DX code is correct then send an appeal to insurance.
Mock Call Questions:
1. What is the status of the claim?
2. When did the claim get denied?
3. Do you need the medical necessity letter or the medical records to process the claim?
4. What is the address to submit the medical necessity letter /medical records?
5. What is the appeals’ address?
6. What is the appeals’ filing limit?
7. Can you fax me a copy of the EOB please?
8. May I have the claim number please?
9. May I have the call reference number please?.
Notes format:
DOS 04/10/2022 as per review found the claim with billed $100.00 was submitted on 04/15/2022 and no response received yet, Called payer UHC @ 888-824-3420 spoke with Sandy and stated that the claim was received on 04/20/2022 and denied on 04/25/2022 stating medically not a necessity. Checked billing summary no payment was found previously on this diagnosis code and CPT code combination. Therefore, requested a corrected claim address PO BOX 31362 SALT LAKE CITY UT 30895 and the time frame is 120 days from the denial date. Also requested appeal address P O BOX 3 0 5 5 9 ATLANTA GA 33589 and time frame is 90 days from denial date. Therefore, sending this to the coding team for review. Claim# 9966. Call reference# 89957.
I am trying to give my best to you to better understand the Medical billing A, R CALLING subject in a crisp and clear format. Hope I am doing that. If you like please support us by SUBSCRIBING to our YouTube channels V BILLINGS https://www.youtube.com/c/VBILLINGS and VB ENGLISH https://www.youtube.com/channel/UCyVYYc_1c6aCfEgpNO8xYFQ.
