Maximum Benefit Exhausted/Met Denial.
Meaning:
- Some insurance companies limit the dollar amount they will pay per year for certain services or they limit the number of services eligible for coverage per year.
- Patient coverage is active but insurance will not pay since the amount of maximum payable has been reached.
- The current insurance has already enough paid for this patient hence this insurance can’t pay more.
- A service or supply may be limited by dollar amount, duration, or a number of visits.
Claim Adjustment and Remark Codes:
CO119: Benefit maximum for this time period or occurrence has been reached.
Reasons:
This denial can be for many reasons such as:
- Annual Benefit Amount
- Individual Lifetime Visits
- Visit Limit
- Dollar Limit.
Steps to resolve :
- Check the benefit details online or on call – whether the benefit limit is visit-based or amount based.
- Check if there is a balance in the benefit limit. If found request to reprocess the claim. If not, check the system to see if the patient has any secondary insurance.
- If there is no sufficient information provided in the system then go back to the original file in which the patient’s insurance information was received and if there is secondary insurance, the claim can be submitted to the secondary insurance.
- If it does then re-file claims to that insurance.
- If the patient does not have any other insurance, bill the patient for the allowed amount.
Note:
This scenario can be worked upon without calling. We need to call the insurance only to reprocess the claim or we are unable to check eligibility online.
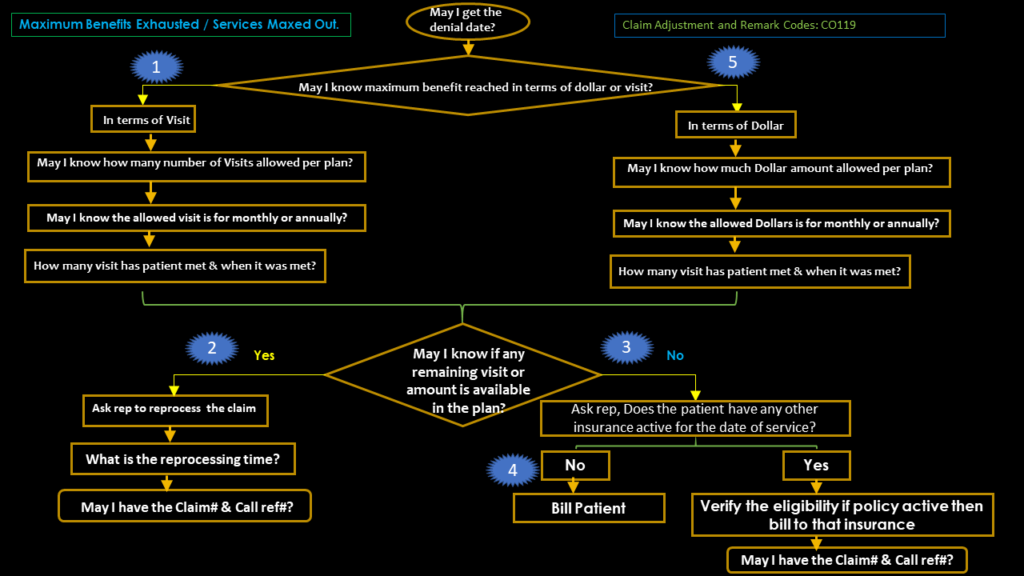
AR Calling Flow chart for Maximum Benefits Exhausted / Services Maxed Out.
Mock Call Questions for MAXIMUM BENEFITS MET denial.
- Can I have the denial date, please?
- May I know if the claim was denied based on the number of visits or dollar value?
- (If by a number of visits? )then ask May I know the total NUMBER of visits for the calendar year, please?
- (If by dollar value? )then ask May I know the total dollar value for the calendar year, please?
- Was the claim processed in-network or out of network?
- When the patient has exhausted these benefits?
- Does the patient have any other insurance active for the date of service?
- Can I have the name of the other insurance and their ID number?
- Can you please fax me a copy of the EOB?
- May I have the claim number, please?
- May I have the call reference number, please?
End action:
- If a patient policy is active for secondary or consecutive payers on DOS then bill the claim to that insurance.
- If no other payer is active or available on DOS then release the claim to the patient.
Notes format:
DOS 04/10/2022 as per review found the claim with billed $1500.00 was submitted on 04/15/2022 and no response received yet, called payer UHC @ 888-824-3120 spoke with Sandy stated that the claim was received on 04/20/2022 and denied on 04/25/2022 stating maximum benefits has been met. Verified about maximum benefits in terms of dollar or visit rep said max benefits reached in terms of visits. Asked the rep how many visits were allowed per plan, the rep said 12 visits were allowed per calendar year and the maximum visits were met on DOS 1/3/2022. Requested the EOB through fax and it will receive in 24 hours. Claim# 558. Call reference# Sandy10/15/2022.
