Claim denied for Prior authorization
Meaning: The insurance does not find authorization for the treatment denied.
Claim Adjustment and Remark Codes:
| CO197 | Precertification/authorization/notification absent. |
| CO198 | Precertification/authorization exceeded. |
| CO15 | The authorization number is missing, invalid, or does not apply to the billed services or provider. |
| CO62 | Payment denied/reduced for absence of, or exceeded pre-certification/authorization. |
Reasons:
- The provider has given the treatment without obtaining the authorization from the insurance
- The treatment is an emergency treatment
- The hospital has already obtained authorization for the same treatment.
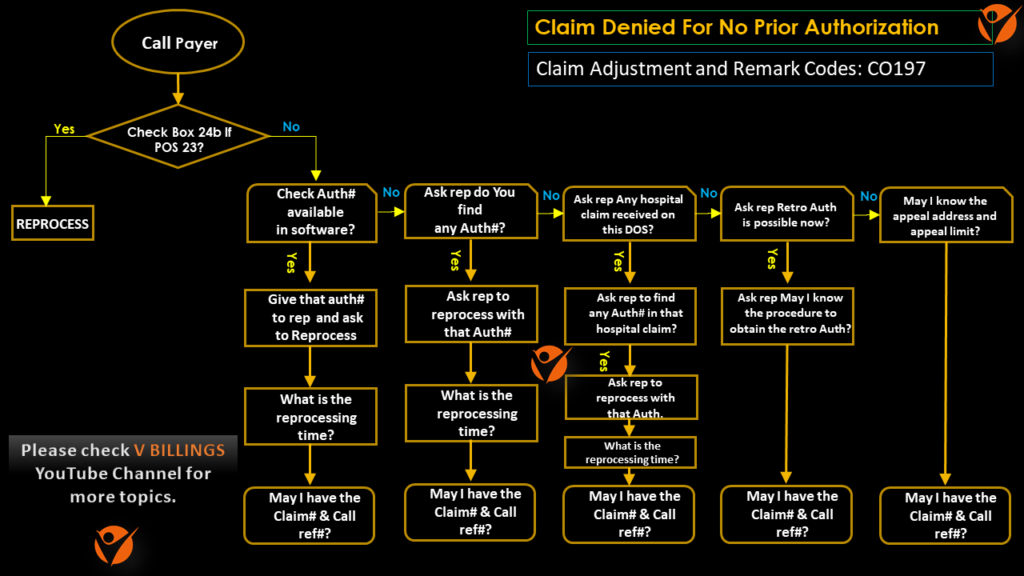
Steps to resolve :
- Check whether the POS is ‘23’. If yes, need to call the insurance and request reprocessing.
- Check whether the POS is ’21’. If yes, need to call the insurance and verify whether the hospital claim has a pre-certification number.
- If the POS is anything apart from ‘23’ or ’21’, need to check whether our billing software has a prior authorization number updated. If yes, need to call insurance and verify that prior authorization number with the payer rep and also try to reprocess on-call.
- If the prior authorization number is not valid or it is not updated in the billing software, need to enquire the insurance if they can accept a retro-authorization.
- If there is no authorization number and a retro authorization is not accepted, then get the appeal address and appeal limit from the payer rep and assign it to client assistance for further action.
Note:
This scenario would need calling.
AR Calling Flow Chart for No Authorization On File.
End Action:
- If there is no authorization number and a retro authorization is not accepted, then send an appeal with complete medical records.
- If the appeal is still denied then write off the claim.
Mock Call Questions for No Authorization On File:
- May I know the claim denied date?
- (If Auth is available in the system)Can you please verify the authorization that I have on file?
- Is that valid for this date of service?
- (If POS is 23) Can you please reprocess the claim as the service is related to an emergency and it does not require authorization?
- (If POS is 21)Do you have a hospital claim on file for this patient and the date of service?
- Can you please use the hospital authorization to process this claim?
- (POS other than 21 & 23) Can we get a retro Authorization for this claim?
- (If yes)Can I have the address and the telephone number of the Utilization Review department?
- (If no retro possible)May I have the appeals address?
- What is the appeals filing limit?
- Can you please fax me a copy of the EOB?
- May I have the claim number, please?
- May I have the call reference number, please?
Notes format for No Authorization On File:
| Scenario | Scenario Description | Notes Documentation |
|---|---|---|
| 1 | Authorization# invalid/missing for DOS, POS code not “23” or “21”. Retro authorization acceptable. | Called Aetna @ 1-800-679-4579. Spoke to rep Cynthia. Rep said that the claim with DOS 12/05/2019,charge $200.00 was denied for prior authorization.Clm was denied on 01/01/2020. Both CPTs 92134 and 66982-50 were denied for authorization. Claim received on 12/30/2019.The prior auth# 6089750 was not valid for the DOS. The POS code was found to be “24”. Rep informed that retro authorization was accepable. The corrected claim filing limit was 120 days from date of denial and the corrected claim could be submitted electronically to the payor id 88451.Got the UMR contact# as 1-800-679-4598. Requested for a copy of the EOB to be faxed @ 1-800- 123-1234 (Attention: Dr.Daniel Brown). Contacted the UMR and got the retro auth# for the as 6595472.Updated the retro auth# and filed a corrected claim electronically. Claim# 123456789. Call ref# A123456. |
| 2 | Authorization# invalid/missing for DOS, POS code not “23” or “21”. Retro authorization not acceptable. | Called Aetna @ 1-800-679-4579. Spoke to rep Cynthia. Rep said that the claim with DOS 12/05/2019,charge $200.00 was denied for prior authorization.Clm was denied on 01/01/2020. Both CPTs 92134 and 66982-50 were denied for authorization. Claim received on 12/30/2019.The prior auth# 6089750 was not valid for the DOS. The POS code was found to be “24”. Rep informed that retro authorization was not accepable. Requested for a copy of the EOB to be faxed @ 1-800- 123-1234 (Attention: Dr.Daniel Brown). Raised a client review task for further action. Claim# 123456789. Call ref# A123456. |
| 3 | Authorization# invalid/missing for DOS, POS code “21”. Hospital claim has precertification#. | Called Aetna @ 1-800-679-4579. Spoke to rep Cynthia. Rep said that the claim with DOS 12/05/2019,charge $200.00 was denied for prior authorization.Clm was denied on 01/01/2020. Both CPTs 92134 and 66982-50 were denied for authorization. Claim received on 12/30/2019.The prior auth# 6089750 was not valid for the DOS. The POS code was found to be “21”. Rep informed that the hospital claim had a precert# . Requested the rep to process the claim with precert# on the hospital claim. The processing would take 15 bsuiness days. Need to follow up after 20 business days. Claim# 123456789. Call ref# A123456. |
| 4 | Authorization# invalid/missing for DOS, POS code “21”. Hospital claim does not have a precertification#. Retro authorization acceptable. | Called Aetna @ 1-800-679-4579. Spoke to rep Cynthia. Rep said that the claim with DOS 12/05/2019,charge $200.00 was denied for prior authorization.Clm was denied on 01/01/2020. Both CPTs 92134 and 66982-50 were denied for authorization. Claim received on 12/30/2019.The prior auth# 6089750 was not valid for the DOS. The POS code was found to be “21”. Rep informed that the hospital claim does not have a precert# and retro authorization was accepable. The corrected claim filing limit was 120 days from date of denial and the corrected claim could be submitted electronically to the payor id 88451.Got the UMR contact# as 1-800-679-4598. Requested for a copy of the EOB to be faxed @ 1-800- 123-1234 (Attention: Dr.Daniel Brown). Contacted the UMR and got the retro auth# for the as 6595472.Updated the retro auth# and filed a corrected claim electronically. Claim# 123456789. Call ref# A123456. |
| 5 | Authorization# invalid/missing for DOS, POS code “21”. Hospital claim does not have a precertification#. Retro authorization not acceptable. | Called Aetna @ 1-800-679-4579. Spoke to rep Cynthia. Rep said that the claim with DOS 12/05/2019,charge $200.00 was denied for prior authorization.Clm was denied on 01/01/2020. Both CPTs 92134 and 66982-50 were denied for authorization. Claim received on 12/30/2019.The prior auth# 6089750 was not valid for the DOS. The POS code was found to be “21”. Rep informed that the hospital claim does not have a precert# and retro authorization was not accepable. Requested for a copy of the EOB to be faxed @ 1-800- 123-1234 (Attention: Dr.Daniel Brown). Raised a client review task for further action. Claim# 123456789. Call ref# A123456. |
| 6 | Claim incorrectly denied. | Called Aetna @ 1-800-679-4579. Spoke to rep Cynthia. Rep said that the claim with DOS 12/05/2019,charge $200.00 was denied for prior authorization.Clm was denied on 01/01/2020. Both CPTs 92134 and 66982-50 were denied for authorization. Claim received on 12/30/2019.The prior auth# 6089750 waswas valid between 12/01/2019 and 12/31/2019 and so valid for the DOS.Hence sent the claim for reprocessing. The reprocessing time is 15 business days. Need to follow up after 20 business days. Claim# 123456789. Call ref# A123456. |
MOCK CALL CONVERSATION VIDEO (US REP AND AR CALLER) FOR AUTHORIZATION DENIAL.
